65M with fever since 10 days
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
》A 65 year old male patient from mallepalli, nalgonda came with chief complaints of
•fever since 10 days
HISTORY OF PRESENT ILLNESS.
Patient was apparently asymptomatic 2 months back after which he developed shortness of breath which was insidious in onset, grade 1 not associated with orthopnea, no diurnal or seasonal variations.
He complains of fever since 10 days which was insidious in onset, low grade, associated with chills and rigors, evening rise of temperature is seen, alternate day fever .
No complaints of cough, chest pain, chest, tightness, hemoptysis.
no history of vomitings, pedal edema, burning micturition, decreased urine output.
PAST HISTORY
No similar complaints in the past
Not a known case of diabetes,hypertension,epilepsy,asthma,tuberculosis,thyroid disorder.
FAMILY HISTORY
No significant family history
PERSONAL HISTORY
Diet -mixed
appetite-decreased
bowel and bladder movements -regular
sleep-adequate
addictions- alcohol
2 chutta every day since 40 years.
DAILY ROUTINE
Occupation - farmer
stopped working since 7 years
wakes up at 6 am
does his daily routine
drinks tea or milk at 7.30 am
has rice and curry for breakfast at 9 am
lunch at 2 pm
sleeps for 2 hrs
takes tea at 6 pm
dinner at 8 pm
sleeps by 9.30pm.
GENERAL EXAMINATION
patient is conscious,coherent and cooperative
well oriented to time,place and person
thin built and moderately nourished
No pallor, icterus, cyanosis, clubbing, lymphadenopathy,pedal edema.
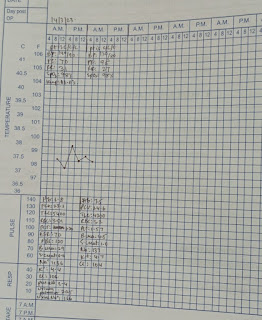
VITALS
BP -110/70 mmhg
TEMP- afebrile
RR-20 cpm
PR- 100bpm
spO2- 98%
SYSTEMIC EXAMINATION
CVS- S1S2 heard, no murmurs
CNS- No focal deficits
PA- soft, non tender
RESPIRATORY SYSTEM
URT:
Nose- no polyps, dns
oral cavity- poor oral hygiene
Post pharyngeal wall- normal
LRT
Inspection
Shape of chest : bilateral symmetrical,elliptical
trachea: central
supra and infra clavicular hollowness
chest expansions equal on both sides
no crowding of ribs
no drooping of shoulders
no wasting of muscles
no usage of accessory muscles of respiration
apical impulse not seen
no scars,sinuses, engorged veins
dry scaly skin seen
no kyphosis ,scoliosis
Palpation:
all inspectory findings are confirmed
no local rise of temperature
no tenderness
trachea central
apex beat left 5th ICS,medial to MCL
TVF increased at right InfarClaviclaruArea, Mammary Area.
diameters
ap: 19cm
transverse: 22 cm
chest circumference: I 79 cm
E 75cm
Percussion
resonant, dullness in right mammary area
auscultation
BAE+
NVBS heard
BBS at right Infraclavicular area
VR increased at right ICA, MA
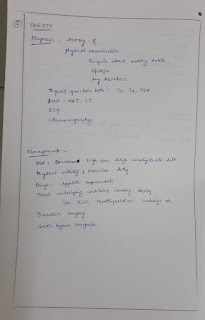
INVESTIGATIONS
CBNAAT positive
Right upper lobe and middle lobe consolidation Secondary to TB
TREATMENT
inj Augmentin 1.2 gm IV TID
inj Pan 40 mg IV OD
inj neomal 100 ml IV
tab PCM 650 mg PO TID
syp aptivate 2 tsp PO BD
monitor vitals,
tab Azee 500 mg PO OD
inj ceftriaxone 1gm IV BD
IVF DNS 500 ml stat
IVF NS 75 ml/ hr
added tab nodosis 500 mg PO BD
protein powder in milk PO BD
started ATT
Tab isoniazid 170 mg PO OD
Tab rifampicin 340 mg PO OD
Tab pyrazinamide 850 mg PO thrice weekly
Tab ethambutol 510 mg PO thrice weekly.


























Comments
Post a Comment