A 48 year old male with fever and uncontrolled sugars
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 48 year old male welder by occupation, resident of cherlapally ,came on 18/6/22 with
CHIEF COMPLAINTS
• Fever since 4 days
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 4 days back and then he developed high grade fever which was insidious, intermittent and associated with chills and rigors and generalised weakness.
Patient also complains of chest pain since 3 days which was on and off and non radiating.
And also diminision of vision.
No complaints of vomiting, shortness of breath, cough, cold, burning micturition, pedal edema.
PAST HISTORY
Patient is a known case of pulmonary TB 4 yrs back.
He developed fever and weight loss 4 yrs back and then he was diagnosed with pulmonary kochs and used ATT for 6 months.
2 months after using ATT, he developed seizures 1 episode and then came to KIMS, Narketpally and then he was diagnosed with Diabetes and is started on Insulin therapy.
Inj.Mixtard 15 IU BD
But patient takes insulin irregularly
He developed tingling sensations in Lower limbs bilaterally since 1 yr and he assumed it was because of night dose of insulin and stopped it voluntarily.
Not a known case of hypertension, epilepsy, asthma.
PERSONAL HISTORY
Diet - Mixed
Appetite - Normal
Bowel and bladder movements - Regular
Sleep - Adequate
Addictions - Alcohol since 20 yrs, occasionally.
GENERAL EXAMINATION
Patient is conscious, coherent and non cooperative .
Well oriented to time, place, and person.
No Pallor
No icterus
No cyanosis
No clubbing
No lymphadenopathy
No edema
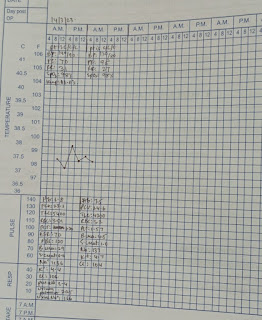
VITALS
BP - 110/70 mmHg
TEMP - 98.6F
RR - 18cpm
PR - 86bpm
Sp02- 98%
**GRBS - 702 mg%
SYSTEMIC EXAMINATION
RS - BAE+, NVBS
PA - soft, non tender, no organomegaly
CVS- S1 S2 heard, No murmurs
CNS - NFD
CHIEF COMPLAINTS
• Fever since 4 days
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 4 days back and then he developed high grade fever which was insidious, intermittent and associated with chills and rigors and generalised weakness.
Patient also complains of chest pain since 3 days which was on and off and non radiating.
And also diminision of vision.
No complaints of vomiting, shortness of breath, cough, cold, burning micturition, pedal edema.
PAST HISTORY
Patient is a known case of pulmonary TB 4 yrs back.
He developed fever and weight loss 4 yrs back and then he was diagnosed with pulmonary kochs and used ATT for 6 months.
2 months after using ATT, he developed seizures 1 episode and then came to KIMS, Narketpally and then he was diagnosed with Diabetes and is started on Insulin therapy.
Inj.Mixtard 15 IU BD
But patient takes insulin irregularly
He developed tingling sensations in Lower limbs bilaterally since 1 yr and he assumed it was because of night dose of insulin and stopped it voluntarily.
Not a known case of hypertension, epilepsy, asthma.
PERSONAL HISTORY
Diet - Mixed
Appetite - Normal
Bowel and bladder movements - Regular
Sleep - Adequate
Addictions - Alcohol since 20 yrs, occasionally.
GENERAL EXAMINATION
Patient is conscious, coherent and non cooperative .
Well oriented to time, place, and person.
No Pallor
No icterus
No cyanosis
No clubbing
No lymphadenopathy
No edema
VITALS
BP - 110/70 mmHg
TEMP - 98.6F
RR - 18cpm
PR - 86bpm
Sp02- 98%
**GRBS - 702 mg%
SYSTEMIC EXAMINATION
RS - BAE+, NVBS
PA - soft, non tender, no organomegaly
CVS- S1 S2 heard, No murmurs
CNS - NFD
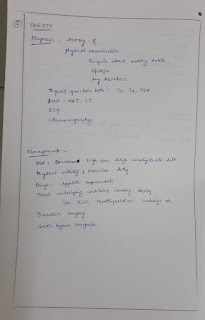
PROVISONAL DIAGNOSIS
Fever under evaluation
Uncontrolled sugars (Type 2 Diabetes)
Diabetic nephropathy?
TREATMENT
IVF NS RL @ 50ML /HR
TAB NITROFURANTOIN 100 mg po BD
TAB .DOLO 650mg po BD
GRBS monitoring
Inj HAI 50 units in 50ml NS IV drip @4ml/hr
Inj PAN 40mg OD
Inj Meropenem 1gm stat
Fever under evaluation
Uncontrolled sugars (Type 2 Diabetes)
Diabetic nephropathy?
TREATMENT
IVF NS RL @ 50ML /HR
TAB NITROFURANTOIN 100 mg po BD
TAB .DOLO 650mg po BD
GRBS monitoring
Inj HAI 50 units in 50ml NS IV drip @4ml/hr
Inj PAN 40mg OD
Inj Meropenem 1gm stat



.jpg)















.jpg)
.jpg)


Comments
Post a Comment